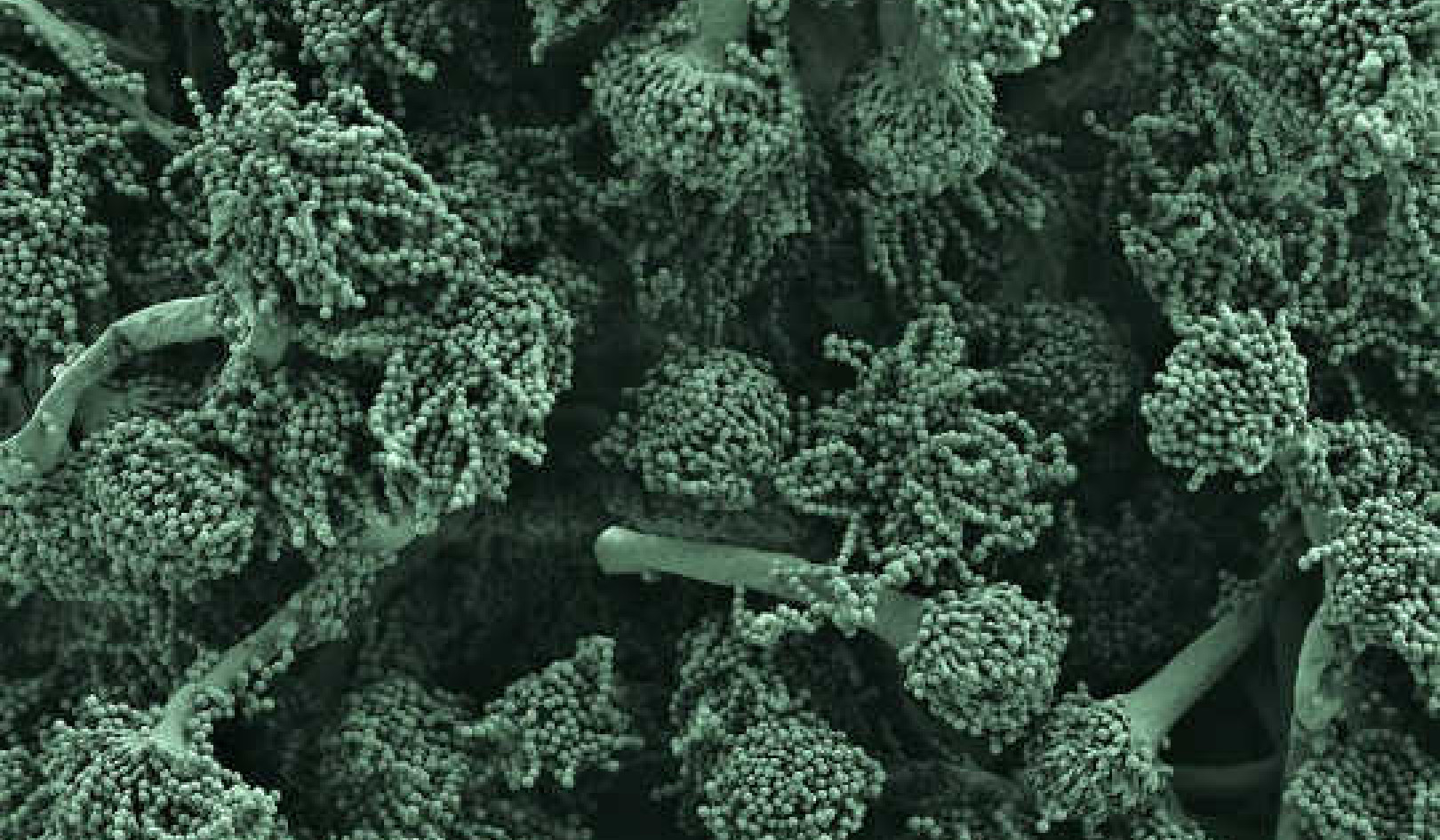
Image by LJNovaScotia
Article medically reviewed by Ioana Bina, MD PhD
Long COVID is a multifaceted disease that can affect nearly every organ system and can manifest as new or worsening chronic health problems, including but not limited to heart disease, diabetes, kidney disease, hematologic issues, and mental and neurologic conditions. The signs, symptoms, and conditions continue or start four weeks or more after the initial (symptomatic or asymptomatic) infection and may be relapsing and remitting (which means the symptoms are at times worse (relapsing) and other times are improved or gone (remitting).
Long COVID is both a personal and an economic problem, as millions of people may be unable to perform their jobs due to their symptoms. Katie Bach, a senior fellow with the Brookings Institution, analyzing survey data from the Census Bureau, the Federal Reserve Bank of Minneapolis, and the Lancet concluded in a conservative estimate that 4 million full-time equivalent workers in the US alone are out of work because of long COVID. This represents 2.4% of the working population.
Do You Have Long COVID?
Roughly twenty percent of those who have been infected report long COVID symptoms, characteristically mood disorders (depression, anxiety), chronic fatigue, shortness of breath, sleep abnormalities, headache, brain fog, joint pains, nausea, cough, and abdominal pain that are particularly apparent during physical or mental stress.
Most people with COVID get better within a few days to a few weeks after infection, so at least four weeks should elapse before post-COVID conditions can be quantified. Anyone who has been infected can experience post-COVID effects. While most “long-haulers” had symptoms during early infection, some people who later experienced post-COVID conditions didn’t necessarily feel ill initially.
Why Long COVID?
The cause of long COVID remains unclear, but some hypotheses are: persistence of virus or viral remnants, autoimmunity, dysbiosis (microbial imbalance), latent virus reactivation, and tissue damage caused by lingering inflammation.
Research is urgently needed to understand the biological mechanisms that underpin the more than 200 symptoms and signs and 50 conditions attributed to long COVID and to develop evidence-based treatments for them.
COVID and the Adrenal Glands
Several ongoing studies have linked cortisol levels with long COVID, owing to the impact of the virus on the adrenal glands. Adrenal gland insufficiency in patients with COVID-19 might be induced through various mechanisms, including vascular damage, viral replication with tissue destruction, inflammatory factors, and improper tapering off of long-term steroid medication.
In addition, the virus appears to use molecular mimicry, a strategy to evade and misdirect the host's immune response, resulting in a breakdown of the normal cortisol response. By way of explanation, our bodies produce antibodies to counter the virus but they react with our own hormone ACTH, which looks similar. So instead of attacking the virus, our antibodies bind with ACTH, which happens to be the releasing hormone leading to the production of cortisol. This is one possible explanation why our cortisol levels drop in long COVID, provoking symptoms indicative of relative adrenocortical insufficiency.
Long COVID symptoms parallel hypocortisolism, a state of paradoxically low cortisol. An article published in Nature in May 2022 alluded to adrenal gland insufficiency developing weeks after infection in patients with COVID-19, either as a direct result of the virus or as a complication of steroid drugs treatment like dexamethasone.
Researchers at Yale School of Medicine in Connecticut and the Icahn School of Medicine at Mount Sinai in New York found that cortisol levels of 99 long COVID patients were roughly half those of the uninfected or fully recovered patients. Fatigue, difficulty with cognition (brain fog), and autonomic nervous system dysregulation were the most common issues up to a year later. Although the study was small, the authors concluded that low cortisol, coupled with increased levels of two proteins (IL-8 and galectin-1) could potentially identify those with long Covid.
Cortisol: The Chicken and the Egg?
It seems cortisol is both the chicken and the egg, with high cortisol increasing the risk of attracting COVID, and low cortisol involved in long COVID symptoms. Several scientific papers were published in 2020 and 2021 about cortisol and COVID:
-
High Cortisol increases the risk of attracting COVID
-
Cortisol as an Independent Predictor of Unfavorable Outcomes in Hospitalized COVID Patients
-
Cortisol as a potential diagnostic factor between recovered and long COVID
Salivary cortisol determination has been recommended in some studies for establishing and monitoring long COVID recovery plans. While this represents great progress, more studies are needed to verify these premises. Hopefully cortisol saliva tests will be validated and allow consumers to test their cortisol levels at home within minutes without the need for a lab.
Bottom line, it’s too early to say for sure that cortisol confirms a long COVID diagnosis, but for now cortisol seems to be the biomarker that’s showing a clear difference between long haulers compared to recovered or healthy people. That’s progress and we’re anxious to see further studies confirming this breakthrough.
Copyright 2022. All Rights Reserved.
Book by this Author
BOOK: Cortisol: The Master Hormone
Cortisol: The Master Hormone: Improve Your Health, Weight, Fertility, Menopause, Longevity, and Reduce Stress
by Wibe Wagemans and Ioana A. Bina, MD, Ph.D. CORTISOL, THE MASTER HORMONE, written by a Ph.D. in endocrinology and a high-tech entrepreneur, is here to explain how you can manage your cortisol levels so your cortisol does not manage you.
CORTISOL, THE MASTER HORMONE, written by a Ph.D. in endocrinology and a high-tech entrepreneur, is here to explain how you can manage your cortisol levels so your cortisol does not manage you.
Working with the research and insights nearly 100 of the world’s best scientists in their respective fields, CORTISOL, THE MASTER HORMONE will help you figure out how to get the data you need to live your best life, and to always understand how your stress levels are impacting your sleep, brain function, blood pressure, bones, gut, appetite, weight, immune system, and aging.
For more info and/or to order this book, click here. Also available as a Kindle edition.
About the Book 's Authors
 Wibe Wagemans is a CEO, serial entrepreneur, and pioneer in mobile and AI technology. He was the first in the world to build an AI bot and an online video game on mobile. Since 2006, he’s been running and advising startups in Silicon Valley, where he built such brands as Angry Birds and Big Fish. His most recent company, Huuuge Games Inc., made its IPO in 2021 for $1.2 billion. He is the founder of Paradigm,Inc., the world’s first company to offer rapid saliva tests to measure cortisol within a few minutes.
Wibe Wagemans is a CEO, serial entrepreneur, and pioneer in mobile and AI technology. He was the first in the world to build an AI bot and an online video game on mobile. Since 2006, he’s been running and advising startups in Silicon Valley, where he built such brands as Angry Birds and Big Fish. His most recent company, Huuuge Games Inc., made its IPO in 2021 for $1.2 billion. He is the founder of Paradigm,Inc., the world’s first company to offer rapid saliva tests to measure cortisol within a few minutes.
Ioana A. Bina, MD, Ph.D. is an integrative medicine physician and board certified gastroenterologist. She is a member of The Institute for Functional Medicine and Academy of Anti-Aging Medicine. She serves on the Scientific Advisory Board of Paradigm, Inc. She is the co-author with Wibe Wagemans of Cortisol: The Master Hormone.
Learn more at Pardigm.com.